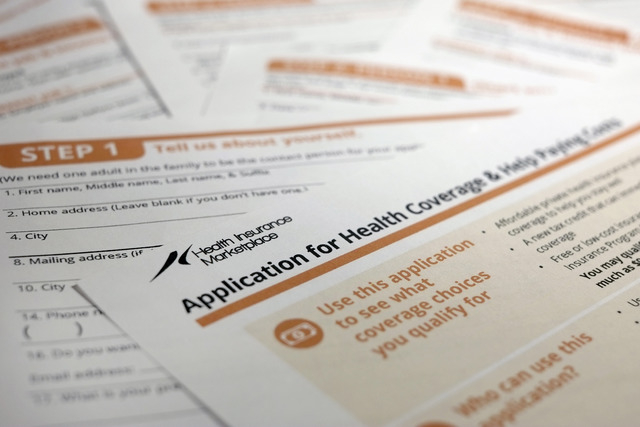
Healthcare choices may narrow for some Nevadans
The Affordable Care Act may put your health insurance network on a diet.
With dozens of coverage mandates taking effect Jan. 1, Nevada’s insurers are looking to control costs by slashing the number of doctors and hospitals they contract with to create what local employee benefits consultants call “skinny networks.” Industry observers disagree on what it means for you: Insurers say leaner networks will improve delivery of care, while brokers say wait times for care will worsen even more than experts already predict.
It’s not clear just how thin those networks might get. Plan designs won’t be available until Oct. 1, when the Silver State Health Insurance Exchange starts selling policies. But early indications show some cuts could be dramatic. One large carrier will roll out a plan with just three Las Vegas-area hospitals in its network, down from the usual dozen, said Michael Caparso, cofounder of National Healthcare Access, an employee benefits firm in Las Vegas. And they won’t be “premier hospitals,” Caparso said.
Plus, where many plans now have 1,800 to 2,000 network doctors, expect to see plans with as few as 500 docs after January.
Not every insurer is trimming networks now, but as large ones scale back, others will follow to compete, Caparso said.
Glenn Shippey, an actuary in the life and health section of the Nevada Division of Insurance, said agency officials are seeing more insurers considering skinny networks in cities, which have thousands of providers. In rural markets, where hospitals and doctors are scarce, it’s less practical.
“In urban areas, there are opportunities for carriers to better control costs with smaller networks, so there’s greater interest in it for that reason,” Shippey said.
There’s more to it than cost-cutting, though, said Christy Daffern, director of operations for Aetna. Aetna will keep plans with fatter networks, and add two plans with smaller networks. An Aetna HMO will partner with all local hospitals except University Medical Center, while its Coventry Health Care of Nevada HMO will work only with HCA Healthcare’s three hospitals, and Valley Health System’s five hospitals. Neither plan will have fewer docs than average, but both will use just one physician practice: HealthCare Partners, a local system of about 300 primary-care providers and 1,700 specialists.
The HMO networks will save consumers as much as 15 percent on premium costs, Daffern said.
Yet, lower premiums won’t mean skimpier care, Daffern said. Aetna calls the coverge a “high-performance network product,” because its smaller provider count allows for easier management and more personalized care, she said.
“‘Narrow network’ has a bit of a negative connotation. With a high-performance network, all of our providers partner to share data, coordinate care and focus on getting members access to the care they need in the right setting at the right time,” Daffern said. “It really helps us with complex case management and on-site hospital reviews.”
Nevada’s biggest insurer, UnitedHealthcare, didn’t comment. The No. 2 insurer, Anthem Blue Cross Blue Shield, said it wouldn’t comment until later this month, when it has firmer plan designs.
Whether you’ll see a trimmed-down network in 2014 depends on your current coverage. If you have a policy through a big company or a self-insured business, and you don’t change plans Jan. 1, your network should stay the same. If you have to change plans, or if you’re buying for the first time, you could see thin networks.
For carriers who offer them, skinny networks save money two ways. First, with fewer providers, consumers won’t seek as much care. If the closest hospital in your network is 20 minutes away, you’re less likely to make an unnecessary trip to the ER, for example. So the networks cut patient-use rates.
They also let insurers carve out the priciest providers. One carrier told Caparso a heart procedure that costs $19,000 at one local hospital runs $43,000 at another. With a skinny network, that carrier can offload the more expensive hospital and cut its reimbursement exposure by more than half.
“In some cases, insurers are looking for the cheapest providers, as long as they’re in good standing, with no violations or Medicare fraud on their record,” Caparso said.
But there’s a flipside to potential savings, Caparso said. Putting thousands of Nevadans into plans with smaller networks could mean long wait times to see a doctor. That could affect quality of care and discourage people from staying in the system. If they have to wait six months for a routine physical, they might decide insurance isn’t worth it, and opt out of coverage.
“There’s going to be a big wave of people entering the health care system, but you’re not increasing providers. In most cases, you’re decreasing providers. People might question why they’re paying premiums, and if they can’t access even the most fundamental services, they’ll get sicker,” Caparso said.
Daffern said Nevada’s acute doctor shortage will create supply issues regardless of insurance networks.
What’s more, given potential savings, it’s important to offer smaller networks for consumers who couldn’t otherwise afford a plan, Shippey said. “If someone is willing to exchange a lower premium for restricted access to broader networks, it could be a good option for them. But it won’t be the only option.”
Contact reporter Jennifer Robison at jrobison@reviewjournal.com or 702-380-4512. Follow @J_Robison1 on Twitter.