Hospitals try to reduce high rate of returns
To follow up on a pediatric emergency case that had resulted in a child's lengthy hospital stay, a nurse from Children's Hospital at University Medical Center phoned the child's young mother after discharge to see how the little one was doing at home.
The mother replied that everything was going pretty well, but she couldn't figure out how to get the powder antibiotic she had received at the neighborhood pharmacy into the syringe so she could then dispense it in her child's mouth.
"The mother didn't understand the medication had to be reconstituted with water before it was drawn up in the syringe," UMC CEO Brian Brannaman said. "The private drugstore assumed she understood, but you can't assume anything, particularly if there is a language barrier. ... Fortunately, with that call we solved a problem that could have resulted in a readmission or worse."
With that example Brannaman was pointing out how challenging it is for a medical center to ensure that patients don't end up back in the hospital, a national problem that again drew attention this week with the release of a report that showed more than 1 million Americans wind up hospitalized again only weeks after discharge -- for reasons that could have been prevented.
"There is so much coordination needed," Brannaman said, noting that patients may have transportation problems that can prevent them from getting necessary medications or to follow-up appointments on time. "The whole community must get involved."
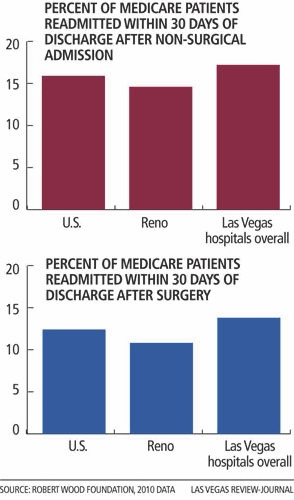
Readmission rates within 30 days for patients in the Las Vegas region -- 13.8 percent for surgical patients and 17.2 percent for patients who had been hospitalized for reasons other than surgery -- were a little more than 1 percentage point worse than the national average, according to the report released by the Robert Wood Johnson Foundation and the Dartmouth Atlas of Health Care on Monday.
"Readmission rates are one of the major quality indicators," Brannaman said, adding that the pressure of insurance companies to keep the length of stay down can result in patients being discharged too soon.
After tiny Boulder City Hospital's 10.4 percent readmission rate for non-surgical patients, UMC's 14.7 percent rate is the best in that category in the Las Vegas area, while Southern Hills Hospital has the worst rate at 19.6 percent.
Summerlin Hospital's 10.9 percent readmission rate for surgical patients is the best in Southern Nevada, and Valley Hospital's 17.6 percent is the worst.
The highest regional rate for 30-day surgical readmissions was 18.3 percent in Bronx, N.Y., with Bend, Ore., lowest at 7.6 percent
The Bronx also had the highest rate for non-surgical readmissions at 18.1 percent, compared with a low of 11.4 percent in Ogden, Utah.
Nationwide, the rate translated to about one in eight Medicare patients readmitted to the hospital within 30 days of being released after surgery in 2010, while patients in for other reasons returned at an even higher rate of one in six. Authors of the report noted that readmissions can happen at any age, not just with the older-than-65 crowd who are counted most closely.
Each year Medicare estimates the readmissions cost $17.5 billion in additional hospital bills.
Anne Weiss, a team director at the Robert Wood Johnson Foundation, said Monday patients and their loved ones must ask questions at hospitals until they understand what they're supposed to do at discharge. She said hospital personnel should ask patients and their families "to repeat what they've been told."
The readmission rates are nearly unchanged from 2008 despite the fact that more than 2,000 ---- around 71 percent of hospitals ---- had been fined up to 1 percent of their base Medicare reimbursements, with hospitals forfeiting more than $280 million in Medicare funds. This fiscal year the fines jump to 2 percent. The penalties, authorized by the 2010 health care law, are part of a multipronged effort by Medicare to use its financial muscle to force improvement in hospital quality.
The government's penalties are based on the frequency that Medicare heart failure, heart attack and pneumonia patients are readmitted within 30 days. Medicare takes into account the sickness of the patients when calculating whether the rates were higher than those of the average hospital.
Valley Hospital, according to Gretchen Papez, a spokeswoman for the Valley Health System, began a Transitional Care Program in 2011 that resulted in a 13 percent reduction in readmissions, or 160 patients, in 2012.
That program brought together representation from nursing, case management, pharmacy, and respiratory and physical therapies.
"We also identify barriers to a successful discharge," she said. "Is there someone who can pick up the patient's medications? Do they have transportation to get to their follow-up appointments?."
She said the entire Valley Health System ---- Valley, Centennial Hills, Desert Spring, Spring Valley and Summerlin hospitals ---- has put the transitional care program into play.
Kristy Bronner of Dartmouth Atlas of Health Care said readmission rates can be a sign people aren't working together.
"Essentially, readmissions are a signal that patients aren't getting what they need when they leave the hospital," she said. She said there are cases in which it's not the hospital's fault that a patient gets readmitted, but "in the aggregate what it shows is a hospital's failure to coordinate post-discharge care so patients don't end up back in the hospital."
Bronner's colleague researcher Chiang-Hua Chang stressed that "case management is extremely important."
Anne-Marie Audet, vice president and health system quality and efficiency at The Commonwealth Fund, a private foundation , said it is not enough that there are caring doctors, caring nurses, caring family members, caring pharmacists.
"If they're not organizing management and services for a particular person, it has significant implications," she said. "Where they fail is where they hand off to one another. The patient doesn't recover as well as he should and it ends up having a significant impact on the cost of care. We can do better."