Need to see a doctor? Just tap the computer mouse
Seeing a doctor in Las Vegas is just a simple mouse click away.
Southwest Medical Associates has turned to telemedicine to treat its patients when they can’t make it to the doctor’s office.
It’s one way Southern Nevada medical practices are turning to technology and collaboration to improve patient treatment and access to medical care. Pediatric Gastroenterology &Nutrition Associates is using a network quality improvement system that involves more than 60 centers in the United States and Great Britain to treat Crohn’s disease and inflammatory bowel diseases.
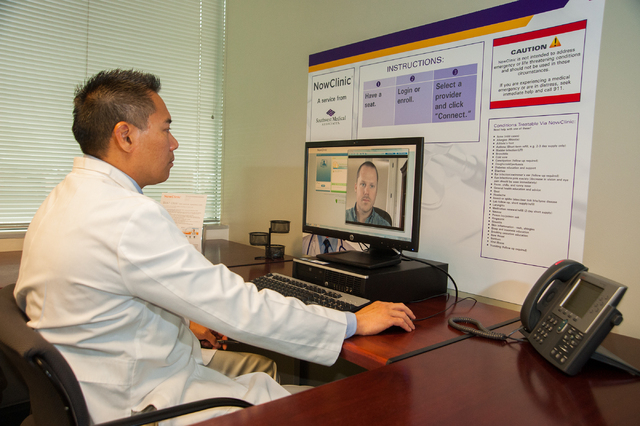
In January, Southwest Medical Associates unveiled its NowClinic technology, which uses telemedicine to improve patient accessibility to care. What started in 2013 a pilot program with employees of Wynn Las Vegas is an option for 325,000 members of Health Plan of Nevada who are eligible for the benefit.
So far 10,000 of those members have signed up. And Southwest Medical Associates, which has five urgent care centers and four walk-in clinics in Southern Nevada, has treated more than 1,500 patients through the first 4½ months of the NowClinic.
It enables patients to access medical care 24/7 without an appointment. It uses Skype-like technology to let patients visit virtually with medical staff by using computers or mobile devices. The appointment can also be done over the phone.
Rather than going to urgent care or emergency rooms or trying to set up an appointment, the telemedicine program is what health plans across the country are setting up and implementing, said Eugene Somphone, Southwest Medical Associates’ medical director.
“There’s a tremendous potential for growth,” Somphone said. “Like any new technology, it takes time. Amazon didn’t become a success overnight, and patients are getting used to this. As they get comfortable, it will be a major avenue for patient care and has huge potential not just in Nevada but across the country.”
The care is limited to wellness, prevention and nonurgent conditions. Those conditions include allergies, asthma, bladder infections, bronchitis, coughs and colds, diabetes, diarrhea, eye infections, fever and chills, flu-like symptoms, high blood pressure, insect bites, insomnia, nausea, rashes, sinus infections, skin infections, sore throats, shingles, and viral illnesses. Patients are able to renew medications and get lab or medication follow-up work.
Patients can talk to a doctor usually within 10 minutes, and the cost is the same as an office co-payment, usually $5 or $10 for most people, Somphone said. An urgent care visit may cost four to five times that amount.
A majority of the patients so far use the service to treat upper respiratory issues, colds, sore throats, bronchitis, bladder infections, allergies and refilling prescriptions, for example, if they’re blood pressure medicine is about to run out before they go to the doctor.
“A classic example would be if you’re a single mother who wakes up with bladder infection and can’t wait. She has two kids and would have to get them up and dressed and take them with her to urgent care and wait to be seen by a doctor. Now, you don’t have to wake the kids and drive down. You can talk with a doctor within 10 minutes and get a diagnosis, and the doctor can send your prescription to your pharmacy for you to pick it up. It’s so simple. This is the best scenario for how this works.”
PEDIATRIC GASTROENTEROLOGY
Pediatric Gastroenterology has participated in the program that employs the science of quality improvement and applies it to medical care.
It starts with meetings every other week between doctors, a nurse practitioner and support staff. The group goes over care, lab works and medication of patients and troubleshoots and doctors take notes to prepare for the patient’s next visit.
“It’s called previsiting planning, and it really kind of makes care that much better,” said Howard Baron, the practice’s senior member. “Rather than pick up the chart off the door two seconds before we walk in, we do our homework and remind ourselves what’s going on.”
After each visit, staff record data into a national database of Cincinnati Children’s Hospital Medical Center – a place renowned for quality improvement efforts, Baron said. The database lists information about bowel patterns, abdominal pain and physician findings. It details lab results and medication doses proscribed and listed whether the patient is in remission, he said.
“All of that data gets sent back to us on a monthly basis on a population management report,” Baron said. “It allows us to manage and entire population. For example, if I choose those with Crohn’s disease ages 5 and 9 with moderate disease, all the patients pop up at once. You can look to see if someone isn’t getting the appropriate doses of medicine and make adjustments. If we see someone that hasn’t visited in six months and is overdue for an appointment, we’ll contact them. It improves efficiency, quality and outcomes.”
Part of this quality improvement process is working with the family and patient self-management to help them learn how to manage the disease and teach them what red flags to look for, Baron said. It lets them know when to call the doctor or nurse and adjust their treatments.