Medical advances helping keep more people with cardiomyopathy alive
Saundra Smith is her normal upbeat self when she shares her experiences with cardiomyopathy. She peppers the recollection with anecdotes and huge smiles. A listener can’t help but marvel at her reaction to what would seem, to most people, a devastating diagnosis: cardiomyopathy with a high risk of sudden death at age 58.
“Gee, my mom never told me how to react when someone says that to you,” says Smith, now 63. “You know, I didn’t want to be rude so I just said, ‘Oh, OK,’” with a polite smile.
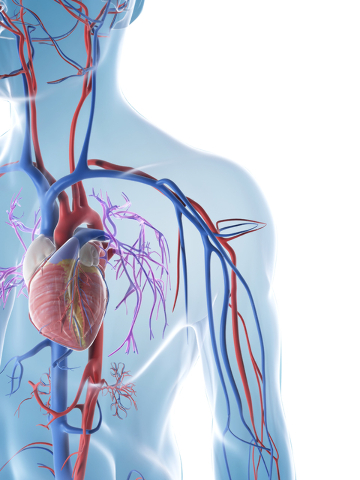
Cardiomyopathy is a leading cause of heart failure and the most common reason for a heart transplant.
Dr. Leo Spaccavento, a local cardiologist says “cardiomyopathy means sick muscle — not necessarily what caused it.”
“Seventy-five percent of the time (cardiomyopathy patients) have had a heart attack — 25 percent of the time, it’s something else,” Spaccavento says.
As the disease progresses, the heart weakens and is less able to pump blood adequately. This can interfere with the heart’s ability to maintain a normal electrical rhythm, which can lead to heart failure or arrhythmia (irregular heartbeats.)
“The problem with heart failure is once it’s caused, it’s hard to reverse,” Spaccavento says. “If it’s a heart attack that you had — you ain’t going to fix that. You’re going to try and prevent any more heart attacks.”
Ignoring subtle symptoms can be fatal.
A dancer since the age of 4, Smith moved to Las Vegas 37 years ago and danced in “Hallelujah Hollywood,” “Lido de Paris” and with Siegfried & Roy.
Always into health and fitness, she was surprised when she began to notice shortness of breath during her almost daily yoga classes.
“If I moved to the left side — I mean doing nothing at all — I couldn’t breathe,” Smith says. “You know, we all kind of just adjust to the situation so when I moved to the left side, I just held my breath.”
It took her doing “this ridiculous thing,” not breathing and holding her breath before she decided to see a cardiologist.
“It took me a while to realize — it wasn’t horrifying, it was just a little weird,” Smith says.
From the time she started to notice the breathlessness until she finally saw a cardiologist was about a year, she estimates.
Looking at the tall, lean, nonsmoker, nondrinker, who never took drugs, the doctor was stumped. But he ordered some standard tests, a treadmill stress test, and an echocardiogram and told Smith she would get the results in two weeks.
But by the time she got home, there already was a phone message from the doctor’s office asking her to come in the next day.
Smith remembers the doctor sounded very calm when he explained his findings.
“It sounded bad, but I don’t think I was really taking in everything he was saying,” Smith says. “I just kept saying (pleasantly) ‘Oh, OK. Oh, OK.’ You know, monosyllabic words — it wasn’t really clicking.”
When the doctor said she needed an angiogram almost right away, he repeatedly told her that she needed to know that she was at a really high risk for instant death.
A few days later as she was being wheeled back to her hospital room after the angiogram, she greeted her husband with a feeling-no-pain drug-induced, “Hi, honey.” But when she heard him on the phone telling their son who was at college in Colorado that his mom would need a heart transplant … “The fog went away instantly,” Smith says. “I was like, ‘WHAT? WHAT?’”
TREATMENT
“If you had a diagnosis of cardiomyopathy before defibrillators, (there was) a 30 percent mortality rate within two to three years,” Spaccavento says.
In 1996, MADIT-I, a landmark study, overwhelmingly showed the life-saving effectiveness of the implantable cardioverter defibrillator (ICD) device in high-risk patients with coronary heart disease. The follow-up study, MADIT-II, showed that prophylactic ICD therapy was associated with significantly improved survival in patients with ischemic cardiomyopathy.
The cardiologist cites advances in identifying markers in blood tests, new drugs and improved implanted defibrillator devices as game changers in the detection and treatment of cardiomyopathy.
“A lot of the new pacing devices have improved survival,” Spaccavento says. “So in the old days you waited for the people to survive (a heart attack) if they were lucky enough. Then you’d put one in. We don’t wait anymore. You basically look for a certain level of heart function. If you don’t go over that number, you get a defibrillator — period.”
Six months after an ICD was implanted in Smith, it saved her life. While on a visit to Colorado, at 3 a.m. she flat-lined in her sleep. The device kicked in and jolted her several times to restart her heart.
“I’ve been very fortunate because it’s never gone off since,” Smith says.
But she was advised to seek out a facility for a heart transplant.
The lead doctor of the transplant program in Arizona took one look at her and asked, “Did you just decide to come here and get a transplant?” Smith says.
“And I said, ‘Can you do that? Can people just decide to have a heart transplant — on a Wednesday?”
The doctor pointed out all the sick people in the waiting room and told her that he didn’t have any patients like her “wearing lip gloss and high heels.”
Smith’s response? “Oh, OK.”
They conducted more tests, readjusted medications and put her on the transplant list — just not at the top of the list. She is doing well — for now — on a new heart medication.
A DESTINATION DEVICE
Dr. Leigh Reardon, director of pediatric mechanical circulatory support and director of the transitional care program for young adults with congenital heart disease at the UCLA Adult Congenital Heart Center, makes the trek to Las Vegas every six weeks for four days to see adult patients at the Children’s Heart Center Nevada.
In April, Reardon presented his innovative research on new heart pump assist devices in Washington at the International Society for Heart and Lung Transplantation’s annual meeting.
“A lot of these patients end up needing heart transplants but oftentimes they are too sick to get a heart transplant or the waiting list is really long,” Reardon says. “Then one of the biggest problems with heart disease is the fact that a lot of people have had multiple surgeries, so the risk of doing a heart transplant is higher.”
A ventricular assist device (VAD) that takes over the pumping function of the heart can be placed in patients waiting for a heart transplant. In adults it is called destination therapy, Reardon says.
“They can actually live on the device until they pass away,” Reardon says. “In children, it’s only approved as a bridge to transplant.”
REHAB AND SUPPORT
Part of Mariana Pencheva-Yanev’s job as a cardiac rehab exercise physiologist at St. Rose Dominican Hospital, San Martin campus, is to give people hope.
The cardiac program focuses on helping people improve modifiable risk factors such as diet, exercise and stress management. Education is a big part of the program. Understanding the “why” of what has happened to them can seem overwhelming at times, Pencheva-Yanev says.
“If we can meet halfway, they decrease their risk of having a second event by 50 percent,” she says. “They also improve their health by 50 percent, so it’s not about perfection.”
“We encourage people to look forward. What happened cannot be changed,” she says. “We tend to linger in that negative space. The most important part is that you have to learn to be patient with yourself.”
For more than two years, Smith has volunteered for Mended Hearts, the world’s largest cardiovascular peer-to-peer support network. Once a week she visits with 20 to 30 Centennial Hospital patients with the same things she experienced. She offers support, educational materials and nonfinancial assistance.
Advice everyone can agree on:
Don’t minimize your symptoms; tell your doctor about what you may think are subtle changes in your body; don’t try to diagnose from Dr. Google or blogs; educate yourself from reputable sources.
For more information: www.mendedhearts.org or local contact: Gerard.annabel1@hotmail.com; www.childrensheartcenter.com; American Heart Association, www.heart.org/heartorg/affiliate/LasVegas/Nevada/Home; St. Rose Cardiac Rehabilitation Out-Patient Program, San Martin campus, 702-492-8565.