Robotic procedure leaves smaller ‘cosmetic footprint’
Forty-nine-year-old aquarist and marine biologist Deborah Canestrelli has a job to do. It involves diving into a 50,000-gallon aquarium at the Forum Shops at Caesars and lavishing tender loving care on rays and sharks — hand-feeding them.
The job keeps her active, and it has been her career for 30 years. So, while in the hospital last November, preparing to have a hysterectomy, she was pleasantly surprised by her doctor’s last-minute suggestion. He offered her a robotic procedure that would create an opening via one hole in her body, rather than a few. The prospect of compromising her body a little bit less was attractive.
Having fewer scars was definitely a plus, she says. And, “less places where your body was opened up. Less places for stuff to get in. Or stuff to get out. I prefer that. When you penetrate your skin, you don’t want any infections getting in there.”
Canestrelli discussed the options with her doctor in the hospital and did some quick research on her “handy dandy” little phone.
She already had heard of single-site surgery: Her son had an appendectomy a few years ago by way of one hole. Her mother, who had a medical background, was also present and “all for” the procedure.
The robotic scene in the operating room clinched the deal.
“Intimidating,” she recalls. “But made you feel safe at the same time. It was a pretty crazy looking room. The thing in there with arms coming off of it everywhere. And everybody’s doing their duty and looking like the bridge of a ‘Star Trek’ episode.”
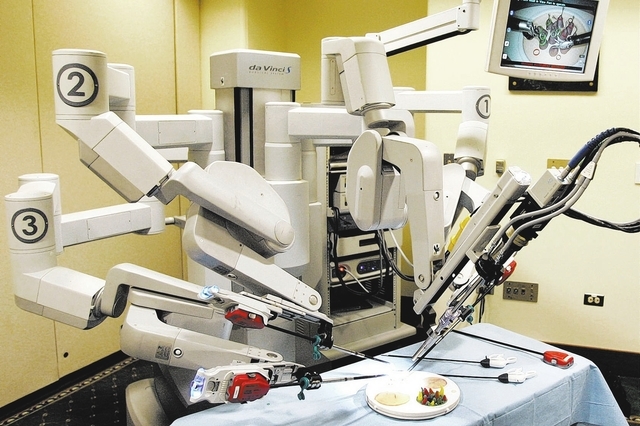
Her doctor brought in OB/GYN Darin Swainston to remove her uterus, via one small incision hidden in the base of the belly button, using the da Vinci Surgical System.
Swainston is director of Minimally Invasive Surgery and Robotics at Summerlin Hospital. He says he was, until recently, the only surgeon performing the procedure in Southern Nevada, although others in the valley are now offering it.
Summerlin Hospital reportedly invested nearly $7 million in a robotic surgical wing that opened last September. It now serves as an observation site for surgeons coming from places such as Arizona, Utah and California to watch and learn from Swainston.
“They come to watch all robotic stuff I do gynecologically,” he says. “But there are more and more now coming to watch single-site.”
Swainston said he is among a handful of surgeons in the country who perform reduced-port robotics. Less than 50 surgeons nationally preside over an observation site, he estimates.
For more than 18 months, he has been proctoring about 30 surgeons. Since September, he has performed approximately 30 single-site hysterectomies robotically.
“It’s about time advances in electronic things are a benefit to women,” he says. “It seems like it’s always a benefit to men. ‘It’s a cool phone!’ ‘It’s a faster car!’ ‘It’s a bigger TV!’ It’s about time that technology is benefiting women’s health.”
Canestrelli can’t see her scar at all, she says, and was able to walk the day after the surgery.
“I never took anything more than Motrin,” Canestrelli says.
After giving her condition a stamp of glowing approval a week after the checkup, her doctor did make her wait five more weeks before returning to work. Back at work, Canestrelli says the only issue she ran into was muscle soreness after weeks of inactivity.
Swainston attributes the quicker recovery time of many of his patients to pre-emptive anesthesia, using local anesthetic agents before making incisions, as the body can perceive pain even while the patient is already “under.”
But, he adds, single-site robotic surgery isn’t necessarily any safer than other options. It is about the “cosmetic footprint” that surgery can leave.
“I had a patient come in today, and I couldn’t believe that we’d done her surgery,” he says. “I couldn’t see any evidence that she’d had the surgery. That’s the benefit of single-site hysterectomy. Because women do care about how they look, and they do care about their abdomen. Especially in Vegas, where the midriff will show, or the abdomen will show, and they don’t want people to see scars.”
Even without robotic technology, single-site surgeries have been around for a long time, according to surgeon Meir Jonathon Solnik, associate clinical professor at Cedars-Sinai Medical Center’s Department of Obstetrics and Gynecology in Los Angeles and the David Geffen School of Medicine at UCLA. He also is the director of Cedars-Sinai’s Division of Urogynecology and Pelvic Reconstructive Surgery, and director of its Center of Excellence for Minimally Invasive Gynecologic Surgery.
Solnik himself performs minimally invasive surgery, which includes robotic surgery. But, while he has taught single-site surgery, he doesn’t use it in his own practice, with or without the help of robotic technology. Both the single-site approach and the robotic platform, may, at best, yield results that are no better than using a traditional laparoscopic approach, he notes.
“I think single-port surgery is not really a prime-time thing,” he says. “It’s more for surgeons who are exceptionally good at laparoscopy to begin with.”
For starters, the single incision using the da Vinci must be even larger than the belly button incision made in a traditional single port surgery.
“You have to be very crafty and artful in how you make the incision, number one,” Solnik explains. “And also how you close it. If you don’t close it well, you could have a pretty ugly-looking belly button.”
And, according to one recent publication he cites, the overall risk of a hernia formation due to the incision may run at about 2.5 percent.
“What that tells me is that if someone knows what they’re doing, the risk of hernia is probably not incredibly high. But it’s still probably higher than the general population. And then, if you add in patients who are at risk for hernias, that risk is not insignificant.”
As for laparoscopic hysterectomies performed with robot versus no robot, “the surgical outcomes are approximately the same, but more expensive with the robots,” Solnik says. “You take someone like me. I’m already well-trained in laparoscopic surgery. Am I going to use the robot for a laparoscopic hysterectomy? No. But if you take someone who is a good abdominal surgeon, knows what they’re doing, but just hasn’t had much experience with laparoscopy, is it going to allow some of those surgeons to do laparoscopic hysterectomy with the aid of this robot? Yes. More women will benefit in that sense. You could argue that maybe we failed in training everybody in laparoscopy. But it behooves us to acknowledge that there are devices that can help us do things better.”
The Food and Drug Administration has received 8,451 medical device reports associated with the da Vinci Surgical System in the past 10 years. Two percent of those involved death, although FDA press officer Jennifer Rodriguez says establishing a cause-and-effect relationship can be difficult. Most of the reports involved component breakage and imaging problems, according to an FDA document, which attributes a rise in those reports to factors as simple as increased use of the robots. After investigation, the FDA last March cleared the robot for marketing.
One possible preferable alternative to the single-port hysterectomy, in general, according to Solnik, is minilaparoscopy, involving even tinier incisions than those used in the traditional laparoscopy.
Another, according to physician Barbara Levy, vice president for health policy at the American College of Obstetricians and Gynecologists, is the vaginal hysterectomy, in which surgery is done by making incisions at the top of the vagina, with none through the abdominal wall at all.
“That’s the least invasive, and the approach with the lowest complication rate,” she says.
But there is a problem with that approach, too, according to surgeon Christopher Tarnay, associate professor of obstetrics and gynecology and urology, and chief of the Division of Female Pelvic Medicine and Reconstructive Surgery in Obstetrics and Gynecology at UCLA.
Tarnay, who teaches robotics relating to gynecology and pelvic reconstructive surgery, says many women aren’t good candidates for the surgery, whether it’s because of a large uterus, scarring from a previous surgery, or because they’ve never had a baby.
Moreover, not all surgeons may be up to the skill level required for a vaginal surgery.
In his opinion, says Swainston, his approach offers big advantages for both patient and surgeon.
“I can see in full 3-D, magnified in high definition,” he explains. “Tell me that is not a benefit when you’re operating inside of somebody.”
In contrast with traditional laparoscopic surgery, the robot also offers him better wrist action and the perspective of being “inside” the patient, sitting on their tailbone with his arms right where they would be naturally if he were doing an open surgery — a “marriage” of the benefits of open and laparoscopic surgery.
Plus, the robotic approach diminishes surgeon fatigue and the likelihood of making mistakes, allowing the surgeon to sit at a comfortable console with arms rested and head rested inside of the console.
“Surgery’s hard on physicians physically,” Swainston says. “It’s theorized that a surgeon can extend their surgical life longer, and that’s very important to patients. Because the longer we operate, the better we get.”
As for complications with the new technology, Swainston recalls a time 20 years ago when surgeons didn’t believe in removing gallbladders laparoscopically.
“We’re implementing a new technology again, and it won’t be the last time.”