Las Vegas mom, diagnosed with cancer while pregnant, is a survivor
Fear kept Nina Santos from saying anything, fear for the life growing inside her, fear for her own life.
She felt the lump in her right breast growing, but she was afraid of what the changes meant. Twenty-eight weeks into her first pregnancy, her denial and attempts to ignore the problem caught up with her, and she heard the three words dreaded by anyone, let alone a woman experiencing the most joyful time of her life: “You have cancer.”
Just 10 years ago, Nina’s story might have ended in tragedy. Doctors often presented expectant mothers with a horrifying choice after cancer was diagnosed during pregnancy: either abort the fetus or delay treating the malignancy until the baby was born. In most cases, the woman, already developing all the feelings of motherhood, including the desire to protect her child at all costs, would choose the latter. Such a decision sometimes resulted in the mother’s death, leaving an inexorable void in the family.
Today, treatments for a pregnant woman diagnosed with cancer have advanced so she can to take her fetus closer to term with acceptable risks to herself or her unborn child. Diagnoses of cancer during pregnancy remain rare, about one in 3,000 women, according to the American Cancer Society. The incidents present formidable challenges for doctors, however, because the condition often is overlooked.
“There are multiple options available,” said Dr. Brian Lawenda, a radiation oncologist at 21st Century Oncology of Las Vegas. “Women do just as well in terms of outcomes based on the age of the woman and the stage of the breast cancer whether they’re pregnant or not.”
Nina, 31, was one such woman, and her story of triumph also provides a cautionary tale for all women, not just those with child, to investigate lumps in their breasts and report to their doctors if they persist for more than a month.
“Don’t ignore a lump,” said Dr. Paul Michael of the Comprehensive Cancer Centers of Nevada, the oncologist who directed Nina Santos’ chemotherapy treatments. “Once women are able to self-diagnose and detect a lump, that obviously means the lump is big enough to have been there awhile. If a pregnant woman waits too long, even a couple months, it can turn from local to metastatic.”
Nina knows that lesson, and she will be thinking of her doctors along with the many reasons she has to be grateful on Thanksgiving. As Nina holds her baby in her arms and reflects on a year of extreme changes and challenges, the new mom cherishes what matters most: family, health, happiness, life.
“After all I’ve been through, she’s my little blessing,” she said.
lump detected a year earlier
A year ago, Francis and Nina Santos were celebrating all the joys of being newlyweds and expectant first-time parents. The couple, who had started their relationship three years earlier after meeting through mutual friends, had been living together since 2012. They were thinking of ways to prepare their three-bedroom home in southwest Las Vegas for the arrival of their baby in the summer.
With no other complications to the pregnancy, Nina was not overly concerned with the lump that she had first noticed a year earlier. She knew certain changes would occur during pregnancy.
In February, the lump had grown enough that she told Francis. In March, the lump was noticed by her obstetrician, Dr. Amit Garg of Women’s Specialty Care in Las Vegas. An ultrasound confirmed Garg’s suspicions, and Nina was referred to Dr. Souzan El-Eid, a breast surgeon with Comprehensive Cancer Centers.
In early April, El-Eid performed a biopsy on the lump, an invasive procedure to remove living tissue for diagnostic evaluation. A biopsy is the only way to make a definitive diagnosis for most types of cancer. Within days of the procedure, the Santoses were called to El-Eid’s office.
“We already knew there was something wrong,” Francis Santos said. “We just didn’t want it to happen while she was pregnant.”
After hearing those three awful words, the pregnancy turned into an obstacle course featuring El-Eid and Michael as her primary oncologists, and Garg and Dr. Brian Iriye, a maternal-fetal medicine specialist with High Risk Pregnancy Center, directing her obstetric care. The first physical effect Nina felt happened when her belly became noticeably bigger after steroids were administered in late April ahead of her chemotherapy.
Until only a few years ago, concern about potential injury to the fetus precluded the use of chemotherapy during pregnancy, but recent studies have shown that some chemo drugs can be used without increasing the risks for birth defects.
In early May, Nina received her first dose of chemo, which she tolerated better than she had expected. Chemotherapy often causes nausea coupled with fatigue and weakness. For Nina, as with many patients receiving chemotherapy, an additional shock came as her hair began to fall out.
Iriye and Garg planned for delivery of the baby about two weeks after the first round of chemo, but the fetal lung development was too immature. Nina’s medical team decided the risk would be minimized to mother and baby collectively to wait. After two more weeks, on May 27, five weeks before her due date, Nina came to the hospital to be artificially induced into labor.
Three days later, after her labor failed to progress adequately, Iriye and Garg recommended delivery by cesarean section.
And on May 30, 2014, at 1:43 p.m., Olivia Ayessa Santos was born at 6 pounds, 1 ounce, and 19 inches long. The staff of Spring Valley Hospital had been advised to prepare for Olivia to spend time in the neonatal intensive care unit, but she was healthy enough that she bypassed the NICU and went straight with Francis to the post-partum unit where she was joined later by Nina after her recovery from surgery.
The baby, with a formidable shock of hair, came into the world in contrast to her mother, who had lost all of hers.
Despite her arduous labor and delivery, the toughest time for Nina was yet to come. Two weeks later, still recuperating from surgery, Nina underwent her second round of chemo, a shock to her system unlike anything she had ever endured.
“After that treatment, I couldn’t even hold her because I was so weak,” Nina said. “My body was not ready yet, because I was still recovering from the C-section. When I started chemo again, it was heavy, especially in my legs.”
Four more treatments over the summer kept the cancer under control, but additional treatment always is recommended so doctors can be sure the malignancy will not return. Nina eventually decided to have a double mastectomy surgery to remove all breast tissue to prevent the recurrence of cancer.
She underwent that procedure in early November, which earned her a new date on the calendar to mark each year: Nov. 11, the day she was declared cancer free.
‘people are afraid of cancer’
Nina’s reluctance to say anything about the lump is a pattern oncologists and other medical professionals understand deeply.
“Breast cancer is a feared diagnosis,” Michael said. “People are afraid of cancer, and if they think something is going on, they delay, they delay, and they delay because they’re so fearful.”
Woman are taught to expect changes in their breasts during pregnancy: growth and enlargement, tenderness and hypersensitivity. Hormones and increased blood supply can affect the pigmentation of the skin and darken the nipples, areolas and the veins along the breasts. As the body prepares the breasts for lactation, milk ducts grow and stretch as they fill early in pregnancy.
“What happens is these women may have a tiny, undetectable breast cancer, and then all of these hormones are dumped into their system, and it revs up the cancer,” Michael said. “Pregnancy is not a risk factor for getting breast cancer, but it can accelerate cancer that’s already there.”
The end result often means a delay in a cancer diagnosis during pregnancy.
“That delay, plus the fact that younger women tend to have more aggressive breast cancers in general, leads to a slightly worse prognosis and outcome,” Lawenda said.
A malignant breast lump removed with surgery requires followup radiation therapy to remove any of the cancer cells that might remain. For years, radiation oncologists were reluctant to use such therapy during pregnancy because of the risk for birth defects. Recently, however, medical researchers have added to data extrapolated from studies of people exposed to radiation during the atomic bomb detonations in Hiroshima and Nagasaki, Japan, at the end of World War II, Lawenda said.
“That’s where all the initial data came from,” he said. “We knew we could do radiation therapy, but we weren’t absolutely sure about the long-term data.”
Some radiation specialists now are confident they can minimize risks early in a pregnancy because the fetus is far enough away from where the radiation is applied to the chest, Lawenda said.
The amount of radiation needed to treat cancer is “orders of magnitude, hundreds into thousands of times greater” than the amount used during a mammogram or X-ray, Lawenda said.
“For the first two trimesters, the fetus is low enough. As the fundus, the top of the uterus, gets closer to the radiation field, we can’t do it anymore,” he said. “After we get to the third trimester, radiation is not recommended, and we have to wait until after delivery.”
Two of Lawenda’s patients have been treated with that process, but most U.S. oncologists remain unwilling to perform the procedure. Radiation during pregnancy is not the “standard of care” in the United States, according to Dr. Farzaneh Farzin, a radiation oncologist with Comprehensive Cancer Centers.
Nina Santos’ cancer was diagnosed in her third trimester, but doctors thought too much time remained before her delivery date to risk waiting until she went full term. The strategy in hers and similar cases is to kill the cancer cells and arrest any spread of the disease with chemotherapy.
“We were all very uncomfortable waiting another six to eight weeks for the fear of it becoming metastatic,” Michael said. “I was afraid if we waited too much longer that it would have spread.”
The steroids were administered to help the fetus’ lungs develop. Then a chemotherapeutic combination of doxorubicin and cyclophosphamide was administered, which helped stop the cancer cells from growing and caused most of them to die. The goal is to deter the cancer long enough for the baby to be delivered and the mother to recover from the delivery to have the additional treatments necessary to make sure she is cancer free. If the cancer metastasizes, spreading throughout the mother’s body, the chances of her survival decrease exponentially.
Nina’s intervention happened with enough time to result in a positive outcome.
Mother has advice for others
Nina is grateful her doctors presented her with options with acceptable risks to herself and her unborn child. When presented the hypothetical situation today, she admits she does not know how she would have made such a choice.
Lawenda and Michael, likewise, are thankful they practice in a modern era when fewer patients face such dilemmas.
“The majority of women, if asked to choose between their life or their child’s, a vast majority will always want to have a healthy child,” Michael said. “If it means sacrificing their own lives, most of them will say yes.”
And while the expectant mothers’ concern for their offspring is paramount, their own health most often is the deciding factor in ensuring a positive outcome for their progeny.
“We’re always most concerned about what’s best for the mother,” said Iriye, the high-risk pregnancy specialist. “As a general rule, what’s best for the mother is going to be what’s best for the fetus.
“Mothers are extremely valiant. Mothers will do almost anything to protect the babies, even to the extent they disregard themselves.”
Nina’s message to other women is to work past their fears, have faith in their health care providers and be optimistic about their prognosis.
“Stay positive and trust in your doctors,” Nina said. “Believe it’s going to be OK. For me, I prayed all the time. I stayed positive for my baby and my family.”
double mastectomy
Nina wants to ensure a long life with her husband and daughter. To that end, she decided to reduce the risk that she would ever have a recurrence of breast cancer by undergoing a prophylactic double mastectomy and reconstruction. The surgery removes all breast tissue, the site where she is most at risk for the cancer returning.
El-Eid, the breast cancer specialist, says the procedure has become more acceptable since actress Angelina Jolie went public in May 2013 with the news that she was undergoing a double mastectomy and reconstruction because genetic tests showed her risk of getting breast cancer was high.
“She has made my job so much easier,” El-Eid said. “Now we’re able to show that the sex symbol is still a sex symbol with the new breasts. It makes a difference.”
Nina’s husband, Francis, has supported Nina unwaveringly throughout her doctors’ office visits, hospitalization and subsequent treatments. The 31-year-old remains remarkably grounded given his frequent brushes with wealth. Not only does the family reside across Hacienda Avenue from Spanish Trail, home to some of the richest people in the world, Francis routinely watches tens of thousands of dollars rain down on crowds as a marketer for Marquis nightclub inside The Cosmopolitan of Las Vegas.
“You have to keep an open mind, knowing the fact that it’s a hard decision to make,” Francis said of his wife’s choice to have the double mastectomy. “But you’ve got to be there for your family, being positive. But there’s no looking back. Either you go through it or you don’t go through it.”
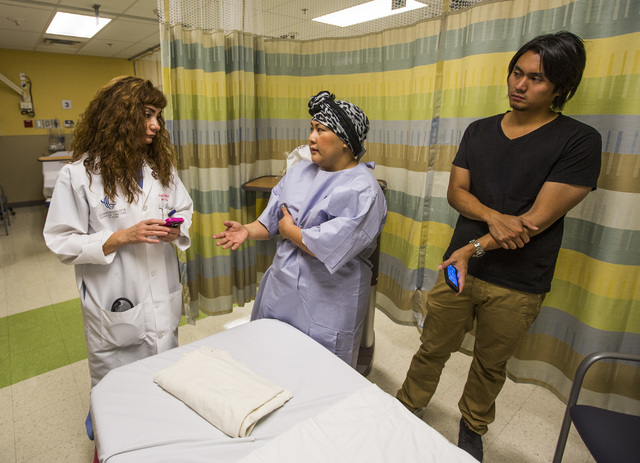
As Nina, her head wrapped in a scarf, was prepped for surgery at Summerlin Hospital in early November, nurses in the preoperative ward repeatedly told her how beautiful she was, voicing the encouragement common in all aspects of cancer treatment.
Positive energy and superior medical care has brought her and her family far, and the journey continues.
“I know I’m in good hands,” she said that day, 30 minutes before the procedure. “I just want to live more. I just want to see my baby grow.”
Contact Steven Moore at 702-380-4563 or smoore@reviewjournal.com.