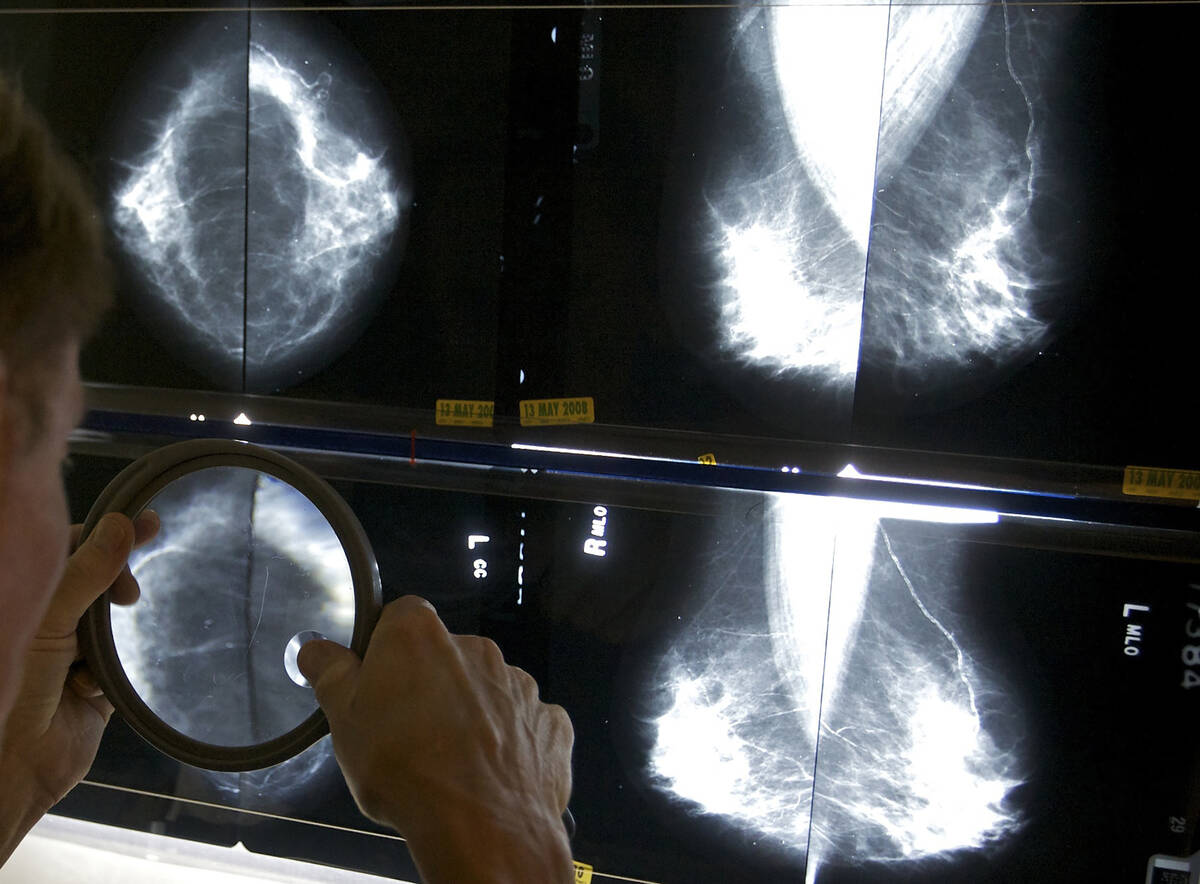
Local breast cancer survivor stresses importance of screenings
Ana Castillo isn’t unfamiliar with the anxiety and challenges that a cancer diagnosis can bring, in part because she’s lost her daughter to brain cancer and her mother to stomach cancer.
But she was “very scared” this year when she learned that she had breast cancer, the 52-year-old Las Vegan says, with daughter-in-law Victoria Vilca acting as translator.
Castillo didn’t know about studies indicating that Hispanic women tend to be diagnosed for breast cancer at later stages of the disease than non-Hispanic women, or that their cancers may be more difficult to treat as a result. And, really, it didn’t matter because she made it a point to promptly receive screening and treatment.
She is continuing her treatment and feels well, Castillo says through Vilca. But she now has a particularly powerful reason to encourage all women — and especially Hispanic women, including her own family — to receive timely breast cancer screenings, Castillo says.
Early detection crucial
A number of studies point to the challenges that Hispanic women face in breast cancer detection and treatment. According to the Centers for Disease Control and Prevention, about 240,000 cases of breast cancer are diagnosed in women annually, and about 42,000 women die from the disease annually.
It is the second-leading cause of cancer death for women overall. And among Hispanic women in the U.S., it’s the leading cause of cancer death, according to the CDC.
Compared with non-Hispanic women, Hispanic women tend to be diagnosed later and with tumors that are larger and more aggressive, making treatment more difficult, says Dr. Arsalan Salamat, director of breast care for Optum Care.
Some of that may involve access to care, “meaning if you’re not getting diagnosed early enough then present at a later stage of disease, at that point the disease is harder to treat and survival rates go down,” Salamat says.
And it’s why regular breast cancer screening — along with better education and having resources to promote screening in the community — is key to improving outcomes, Salamat says, despite socioeconomic and practical barriers to screening that might exist.
For example, some studies show that states that have expanded Medicaid and made mammograms more accessible to women experience increases in mammogram screenings, according to Dr. Stephani Christensen, a medical oncologist with Comprehensive Cancer Centers of Nevada.
Importance of screening
Risk factors for breast cancer include family history, genetics and having dense breast tissue, according to the American Cancer Society. Other risk factors include obesity, consuming more than six to eight drinks weekly, and having used oral contraceptives, Christensen says.
Even childbirth figures into the equation. “If your first childbirth was above age 30 or if you have no children, the higher the risk of breast cancer,” Salamat says.
While reducing the risk of breast cancer involves a mix of factors that can and can’t be modified, one preventative measure remains solidly in the hands of women: receiving timely and regular screenings.
Yet some women tend to put off screening and mammograms. Anxiety about what a mammogram might reveal can cause reluctance to be screened at all, Salamat says.
“I think it does exist,” he says. “I think there are a lot of people who put it off with that fear.
“It’s important on all levels to just get out and inform them of the risks,” he adds.
‘It was worth it’
Castillo had a mammogram last November, and a lump in her breast was discovered. However, “they couldn’t tell it was cancer,” she says through Vilca.
But the lump grew over the next few months, Castillo says, and a cancer diagnosis came in February. She began treatment and completed chemotherapy in July.
“She said that after the chemo she started to eat well and decided to walk around a little more,” Vilca says. “She started gaining weight again.”
Today, Castillo says she’s feeling better and is grateful for the doctors and nurses who cared for her. She’s continuing treatment, which she admits was scary and difficult at times.
“She said it’s worth it,” Vilca says. “It was really hard for her. It was painful, the whole process, but it was worth it.”
According to Salamat, the general recommendation for women of average risk is to begin annual mammograms — preferably the 3D type — at age 40. For women with a family history of breast cancer, screenings will probably begin earlier.
“I’d recommend all women be screened annually over the age of 40,” Christensen says, although modifications to that general guideline may be merited based on family history and personal circumstances.
For example, in the case of a woman who has a first-degree relative with breast cancer, screenings probably would “start 10 years before the first-degree relative was diagnosed,” she says.
‘Make sure you’re screened’
Meanwhile, the backlog of mammogram screenings that occurred during the COVID shutdown has eased, Salamat says, although “I would say we’re still kind of working through it. We’ve done a lot of outreach, particularly among high-risk populations.”
If a lack of health insurance is an obstacle, “there are places that are willing to do screenings and mammograms,” Salamat adds. He recommends consulting the American Cancer Society and the Susan G. Komen Foundation for information.
“They’re great organizations and also nonprofit,” says Salamat, who also recommends consulting your primary care physician.
“The access issue has gotten better,” Christensen says, but “we still have inroads to make. There are ways locally to get mammograms even if you don’t have insurance. Make sure you’re screened.”
Meanwhile, breast cancer treatment options have also advanced significantly in recent years.
“The last 20 years have seen several new drugs that have been developed to treat certain kinds of cancers,” Salamat says, allowing “more personalized” treatments targeting specific cancers.
Pointing to advancements in oncology, Christensen says: “I can think of at least five treatments I use on a weekly basis for breast cancer alone” that didn’t exist less than a decade ago.