450K Nevada residents could lose this federal benefit. Are you on the list?
Thousands of Nevadans could lose their no-cost Medicaid health coverage this year as pandemic emergency provisions wind down, according to state officials.
Following a three-year grace period during the worst of COVID-19, Medicaid recipients will be required to reapply for benefits beginning April 1.
In Nevada, the number of Medicaid recipients swelled by 40 percent during the pandemic under federal emergency provisions that kept states from removing anyone from the rolls, according to state figures. Today, 938,000 people — or nearly one in three Nevadans — receive coverage under the program for the poor and the disabled that in the last fiscal year cost $5.5 billion.
How many Nevadans could be bumped off the rolls?
“That’s the magic question,” said Kelly Cantrelle, deputy administrator for the state’s Division of Welfare and Supportive Services.
She said there are too many variables to be more precise than to estimate possibly thousands.
Some people may be disqualified because they make too much money. But others may lose benefits simply by failing to reapply to the program.
“That’s where we’re concerned that someone could fall through the cracks,” Cantrelle said.
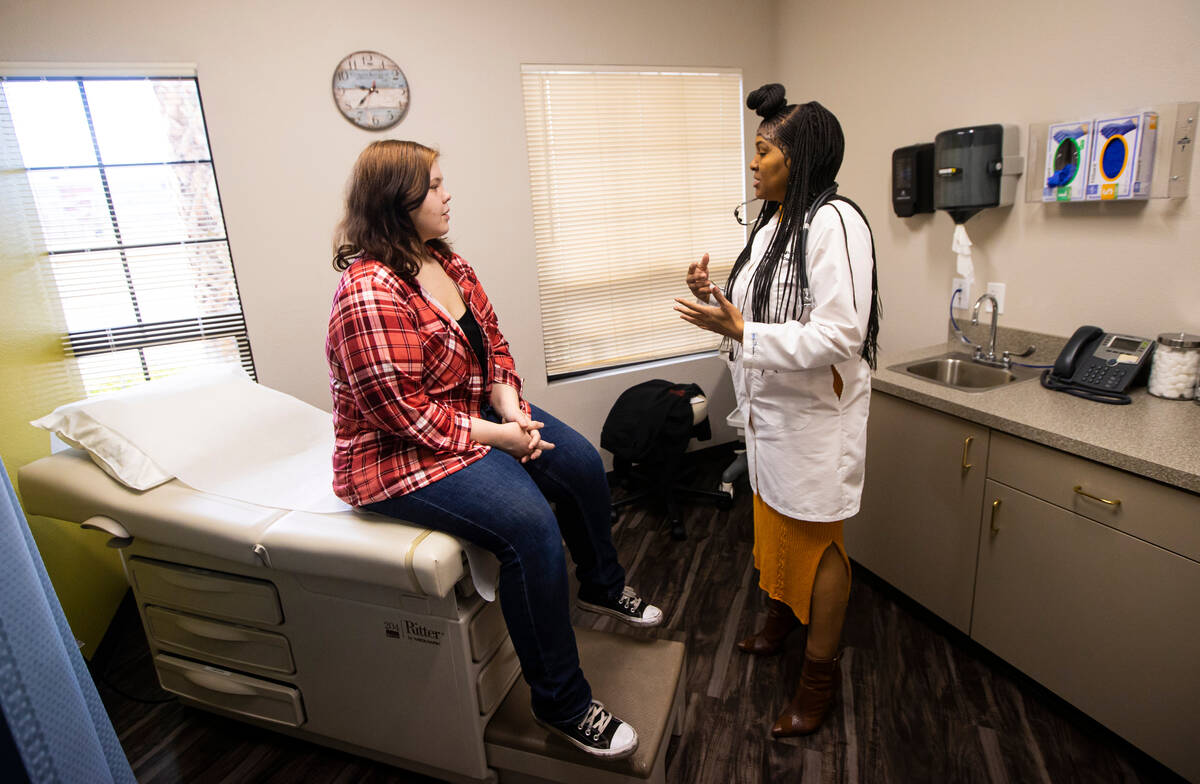
To prevent this, FirstMed Health and Wellness, a federally qualified health center providing primary health care and mental health services in Southern Nevada, is notifying all its Medicaid patients of the requirement to reapply, CEO Angela Quinn said.
The first priority is for a patient to provide an updated address to state Medicaid. After that, “Don’t ignore that letter in the mail, because you could be without health care,” she said.
Although Quinn is confident that FirstMed patients are getting the word, she fears that other recipients have not heard.
“I understand the argument that the consumer needs to educate themselves,” Quinn said. ”But I also understand that these are unsophisticated consumers, and that they have conducted their health care for almost three years one way, and to reintroduce them to the right way is going to take a concerted effort.”
“And I’m not really seeing that from the state yet,” she said.
She would like to see state Medicaid delivering public service announcements that plainly state, absent jargon or technical explanation, that people are at risk of losing their coverage.
“I think it should be really simple: ‘You might lose your coverage. You talk to your provider or you talk to us. Don’t let this happen,’ ” she said.
Cantrelle said a “massive outreach” effort is underway to inform recipients that they need to reapply, including through the food assistance program SNAP, which also serves many Medicaid recipients.
She acknowledged limitations.
“We do not have paid outreach,” she said, meaning her department is not paying for advertisements.
“So we’re doing everything that we possibly can, and part of that is working with our community partners to just get the word out as far and wide as we possibly can,” Cantrelle said.
Medicaid HMOs and health care providers are working to inform their clients, she said.
‘I feel for them’
Individuals making up to $1,677 per month may qualify for Medicaid, while a pregnant woman may earn up to $2,005 a month, according to Julie Balderson Knight, a public information officer with the state welfare division.
The parents in a family of four may receive Medicaid with a household income of up to $3,450 a month. Their minor children can receive coverage if the family’s income is as high as $5,125 as part of a program with a quarterly co-pay.
For those Medicaid recipients who lose eligibility, the “next best option” is to purchase insurance through Nevada Health Link, the state’s insurance exchange, said Ryan High, executive director of the Silver State Health Insurance Exchange.
The exchange is geared toward independent contractors, gig workers, and those whose employers don’t offer health insurance or for whom the premiums would take too big a bite out of their paychecks.
Increased federal subsidies are making health insurance through Nevada’s exchange less expensive than in previous years. Nine out of 10 exchange consumers receive subsidies and tax credits, High said. More than half spend less than $100 per month on premiums.
With Nevada Medicaid rolls ballooning from 671,000 people to 938,000 over three years, High estimated that 100,000 or more Nevadans might no longer qualify for the no-cost program and that some would turn to the exchange for coverage.
“We think we will have some affordable options here to help consumers with their continuous care and continuous coverage,” High said.
Serenity Oliveira, a patient at FirstMed, said she was relieved to learn from the health center that she would still qualify for Medicaid. The 20-year-old, who works part time at a Las Vegas grocery store and has applied for a second job at a fast-food restaurant, said having coverage allows her to continue treatment for bipolar disorder.
“I feel for them,” she said about people who would be losing coverage. “There are people who need it more than I do.”
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.
Resources
To update their address, Nevada Medicaid recipients can visit http://dhcfp.nv.gov/UpdateMyAddress/, call 1-800-992-0900 or visit a local Medicaid office.
For information on purchasing insurance through Nevada Health Link, the state's insurance exchange, visit https://www.nevadahealthlink.com/ or call 1-800-547-2927.