Diagnosing mental issues can be as much art as science
Someone with a mental disorder may be the last person to realize they need help. Often, it’s those around them who notice things aren’t right. Symptoms may include changes in mood, personality, personal habits and/or social withdrawal.
According to the World Health Organization, mental illnesses account for more disability in developed countries than any other group of illnesses, including cancer and heart disease; published studies report that about 25 percent of American adults have a mental illness and that nearly 50 percent of the population will develop at least one mental illness during their lifetime.
“There are clinical criteria that indicate treatment using medications, but that also can be somewhat of a challenge,” said Dr. Jeffery Talbot, director of the Research Center on Substance Abuse and Depression at the Roseman University of Health Sciences. “We often refer to the mental condition not as defined illnesses with defined causes because the symptoms can vary from patient to patient, so it would be fair to say the diagnosis … can be as much art as science.”
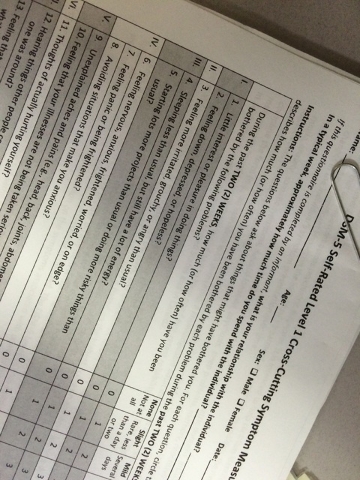
When it comes to diagnosing mental illness, the first clues a clinician gets often come from the Diagnostic and Statistical Manual of Mental Disorders, or DSM-5, compiled by the American Psychiatric Association. The DSM-5 form is filled out by patients on their initial visit.
Questions include: Have you had little interest in doing things?; Feeling, down, depressed or hopeless?; Avoiding situations that make you anxious?; Hearing things other people couldn’t hear, such as voices when no one else is around?; and Feeling detached or distant from yourself, your body, your physical surroundings, or your memories?
Patients can rate the impact of the symptom on their life on a scale of one to four.
One’s medical history will need to be disclosed as will all medications taken. The psychiatrist will then delve further into the person’s symptoms and note when they began.
Local psychologist Dr. Charles Colosimo takes many factors into consideration during the interview: appearance, mood, and whether cognizant functions are operating in the here and now.
“You can’t rely (just on) the DSM-5,” Colosimo said. “You have to get (symptoms) sorted out first of all to see if there’s any medical ideology or neurological ideology, or if there’s been a traumatic brain injury or some outside (trigger), or is it internal. I definitely will try to find out what the situation is that brought them in and how much the crisis or the clinical problem they’re having is affecting their daily functioning.”
Colosimo said personal situations, such as divorce or custody issues, are factors in mental distress.
He added that discerning between issues, such as bipolar and post-traumatic stress disorder (PTSD), in a patient is key.
“You have to figure out what the primary issue is,” Colosimo said. “That’s the one you focus on. If their bipolar has kicked in and caused them to be very unstable, or if they’re having a terrible time, they could not be taking their medication, or maybe they’re not even prescribed medication. All those things have to be sorted out in terms of where you go with it. … If it’s PTSD, you work with it and figure out what the trigger was and how to (treat it).”
He said some physical issues could manifest psychological ones.
“So, we always have to be on top of that,” Colosimo said.
While prescribing medication is often a first step, therapy is important to address the underlying cause.
How long does it take for people to get back on track and on with life? There’s no one answer.
“If someone comes in, and you determine they need therapy, you don’t want to give them four weeks of therapy,” said Patrick Bozarth, executive director at Community Counseling Center of Southern Nevada, 714 E. Sahara Ave. “That’s not going to do anything.”
He estimated that a person would need at least six months of weekly sessions. Group therapy is seen as important because it provides peer support.
One’s position in life can be an indicator of mental challenges. Data from the National Health and Nutrition Examination Survey, 2009-12, shows that those living below the poverty line were nearly two and a half times more likely to have depression than people at or above the poverty level. Sometimes life’s day-to-day drama can bring on bouts of depression.
“We have a higher percentage of mental illness,” Bozarth said of Las Vegas. “I think that has to do with Las Vegas being a transient community. … For so long, we’ve had economic issues that affect the population. The housing crisis that we went through, and that still exists, unemployment, long-term unemployment and the inability to find a decent-paying job — these are all stress-ers that (lead to) anxiety.”
Those with mental health problems can affect the rest of the population, as well.
Bozarth said there’s a cost to society, seen in the panhandlers on the street or erratic driving as people turn to drugs or self-medicate.
“Theft, rape, violent crime can be attributed in part to mental health,” he said, “and certainly substance abuse issues.”
If you or someone you know is in crisis now, seek help immediately. Call 800-273- 8255 or dial 911.
Editor’s Note: This is part of an ongoing story series in View looking at mental health in Southern Nevada.
To reach Summerlin Area View reporter Jan Hogan, email jhogan@viewnews.com or call 702-387-2949.
Support Groups
— The National Alliance on Mental Illness (NAMI) is the largest grassroots coalition for mental health in America. It meets at 6 p.m. Tuesdays in Building 2 at 6161 W. Charleston Blvd. Visit namisouthernnevada.org or email Info@NamiSouthernNevada.org.
— Harmony Healthcare offers adult and adolescent support groups. Before attending a session, verify with your insurance that you are eligible. Call 702-251-8000 or 800-363-4874.
— Nevada 211 offers group therapy on a sliding-fee scale for adults struggling with anxiety, depression and grief. It has two groups in the valley: 220 E. Horizon Drive; email empowermentcentre.change@gmail.com or call 702-565-5004; or at 2121 Las Vegas Blvd. North; visit dpbh.nv.gov or call 702-486-5750.
— Depressed Anonymous is a 12-step recovery group that is based on the model of Alcoholics Anonymous but is designed for recovery from depression and depression-related maladies. It conducts weekly meetings at the Center for Spiritual Living, 1420 E. Harmon Ave. Call 702-739-8200.
— The Depression Bipolar Support Alliance can be found at meetup.com/depression-439 and offers supportive services and activities, including peer-run support groups. It meets at two locations: from 6 to 7:30 p.m. Wednesdays at Rawson-Neal Psychiatric Hospital, 1650 Community College Drive; and from 6:30 to 8 p.m. at Seven Hills Hospital, 3021 W. Horizon Ridge Parkway.
— Victorious Beginnings, a faith-based depression group, meets from 5:30 to 6:30 p.m. Thursdays at Kayenta Legacy, 9418 W. Lake Mead Blvd. Call 702-830-5276.
— Hauva Manookin, MS, CPC intern, offers the SCREAM anxiety education and support group from 6 to 7 p.m. Tuesdays and YANA depression education and support group from 6 to 7 p.m. Thursdays at 2320 Paseo Del Prado, Suite B-111. Call before attending: 702-550-9750.