Las Vegas hospitals add beds, staff to handle spiking COVID cases
Hospitals across the Las Vegas Valley are adding beds and staff to accommodate growing numbers of COVID-19 patients.
“We’re not at danger of being overrun,” said Dan McBride, chief medical officer for the Valley Health System, which operates six hospitals in the valley.
However, he said last week, “These conditions can change quickly.”
By activating their surge plans, hospitals can increase capacity 20 percent or more beyond their numbers of licensed beds. But space is only one piece of the puzzle. Another is staffing.
Acute-care hospitals in Clark County this week had added 441 staffed beds as of Thursday, according to data from the Nevada Hospital Association. Another 49 were added in other parts of the state.
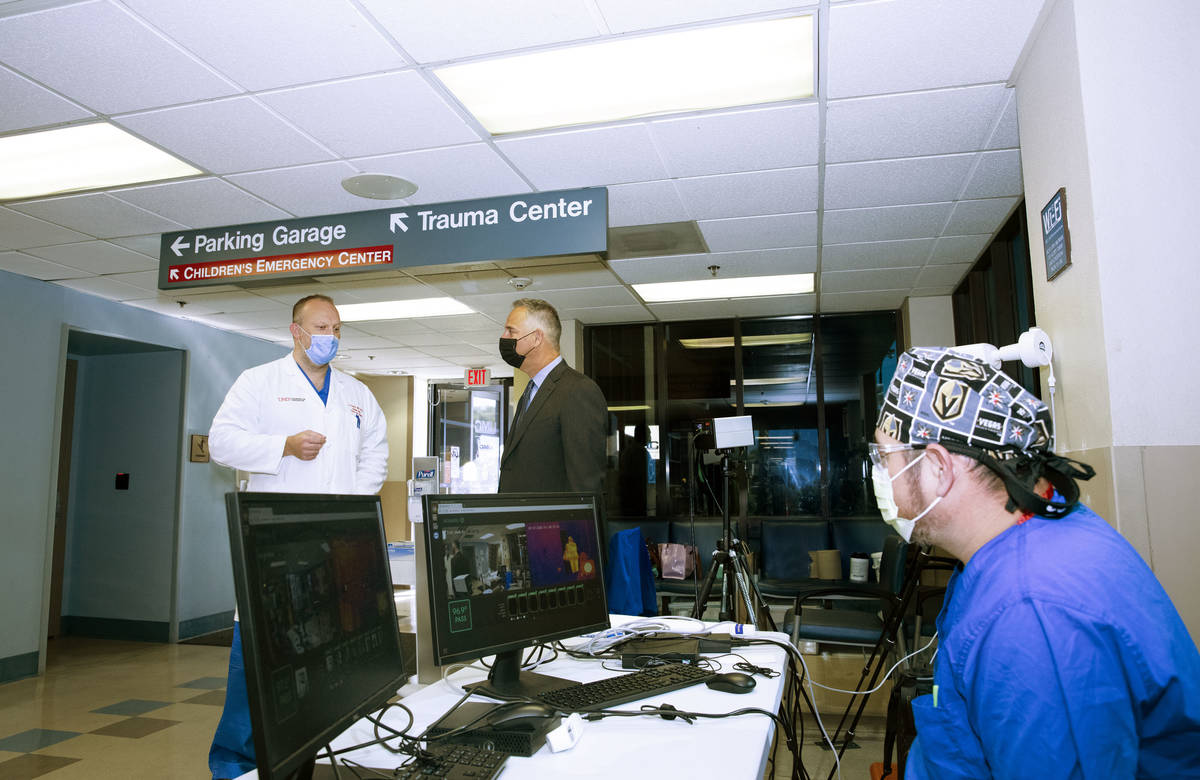
University Medical Center, whose intensive care unit was 95 percent occupied as of Wednesday, added 87 beds by putting under-utilized space to new uses, CEO Mason VanHouweling said.
UMC has increased the age for patients in its children’s hospital to 21 and has put regular patients in the maternity ward to free up space in other areas of the campus. Post-surgical and intermediate-level care areas have been converted into ICU space. Some patients are being kept in the emergency department overnight.
The repurposing of space prompted by the pandemic has been unprecedented.
“Did I ever think that would happen in my lifetime, in my health care career? No,” VanHouweling said. “But our team has made it very safe and have all the right equipment and staffing, and it’s helping us manage through these times.”
Thirty-six percent of patients in UMC’s ICU are COVID-19 patients. The county hospital, which has the state’s only level 1 trauma center, also is treating accident victims as well as patients with heart attacks, strokes and other ills.
At 76 percent, overall occupancy at UMC was slightly higher than during peak periods in the fall and winter, when hospitals are treating high volumes of flu cases, VanHouweling said.
Occupancy rates across the county at midweek was 89 percent of ICU beds, according to hospital association data.
As of Thursday, there was an occupancy rate of 73 percent in the county for all ICU, emergency department, overflow, observational and surge beds at acute care hospitals, according to hospital association spokeswoman Amy Shogren.
Occupancy is not high enough to require activation of a county plan to use the Las Vegas Convention Center to hospitalize patients who require less intensive treatment, said Clark County Fire Chief John Steinbeck. The plan, designed by the Army Corps of Engineers, would provide 900 beds.
‘Biggest vulnerability’
Hospitals are facing another challenge: the need to add staff with the right skills.
During the previous COVID-19 spike in March and April, a key challenge for hospitals was acquiring adequate amounts of personal protective equipment for staff, a shortage that has eased considerably.
In other parts of the country, a shortage of ventilators was another chokepoint, said Dr. Joseph Corcoran, the chief medical officer overseeing HCA Healthcare hospitals in California and Nevada, including the Sunrise Health system’s three Las Vegas hospitals.
“We were able to acquire more ventilators. Some of them have a Ford logo on them. Go figure,” Corcoran said, referencing how Ford Motor Co. began to manufacture the ventilators used to assist patients with breathing.
And now another challenge. “Our biggest vulnerability is staffing — availability of people with the right talent and the right competencies to deliver the right care,” Corcoran said, sharing a sentiment echoed by other hospital representatives. “Talent has to be licensed to practice in the state, which in emergencies, there’s regulatory relief for that. But they also have to have the competencies to practice in that environment.”
“Can you take somebody from labor and delivery and put them into a critical care unit? Some you can, some you can’t. They’re not widgets, right?”
McBride said that nurses treating patients in surgery-recovery areas or in the ER can be shifted to treat patients requiring intensive care. The Valley Health System also has a floating team of nurses that moves among its hospitals to where they’re needed.
Hospital representatives said they employ temporary labor, but they’re now competing with hospitals across the country for this same talent pool, which has led to bidding wars. Some hospital staff members have taken leave to work in other parts of the country for higher pay. Remaining staff members are putting in overtime.
“We are getting closer every day that patients in this community keep getting infected to reaching a limit on where we can’t take patients,” Corcoran said.
He and others interviewed said it’s essential that the community do its part to keep hospitalization rates manageable by practicing social distancing, wearing face coverings and avoiding crowds.
“Get the knuckleheads off of the streets and out of the bars,” McBride said. “And you can quote me on that.”
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter. Review-Journal staff writer Michael Scott Davidson contributed to this report.