Hospital ERs underwhelmed as coronavirus fears keep patients away
A 50-year-old man arrived at a Southern Nevada hospital emergency room complaining of abdominal pain. For three days, he had suffered from what he thought was indigestion, afraid to visit an ER for fear of catching COVID-19. The man had a tear in his bowel that required surgery.
Another man had chest pain for a week before he finally went to an ER. He needed triple bypass surgery.
Situations such as these, where people with serious conditions are delaying seeking medical treatment, are playing out across Southern Nevada.
By delaying treatment, people are jeopardizing their chances for a full recovery and, in some cases, their lives, hospital doctors said this week.
The two men above were treated by the Valley Health System, which includes Valley Hospital Medical Center, where Dr. Jeff Davidson is the medical director of the emergency department.
Davidson said that people with serious conditions should be confident “that we’ve taken all the right precautions so that you can safely be evaluated in our emergency department.”
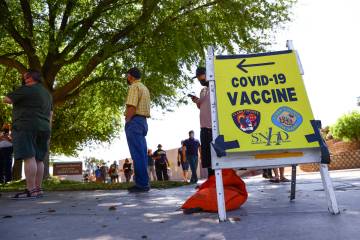
Early in the outbreak last month, public health and government officials in Nevada urged the public to stop going to emergency rooms to try to be tested for the coronavirus unless they were seriously ill. They warned that hospitals could be overrun with COVID-19 patients, as models for the disease progression suggested, if the community failed to “flatten the curve.” People were encouraged to “stay home for Nevada” and to practice social distancing.
The public may have taken the messaging too much to heart. “While we appreciate the public’s response about keeping the ER clear, we don’t want to send the message that it’s only for COVID-19 patients,” said Dr. Dan McBride, chief medical officer for The Valley Health System.
Dangerous delays
Emergency departments in Southern Nevada are isolating suspected COVID-19 patients and requiring them to wear masks to reduce the risk of infecting other patients, among other precautions, said Dr. Derek Meeks, a trustee with the Clark County Medical Society and emergency department director at Boulder City Hospital.
Patient volumes have decreased to the point that hospitals are reducing shifts for ER doctors and nurses, he said. But fear of the ER may be misguided.
“The potential dangers of not going (to the ER) when you need to go are so much greater than the potential for catching COVID-19 while you’re there,” he said.
Chest pain, abdominal pain, trouble breathing, high fever, weakness on one side of the body, a significant new injury or symptom all may be signs of a serious medical issue warranting a trip to the ER, he said. Patients unsure of the severity of their symptoms may want to consult with their doctor or go to an urgent care.
Delaying treatment for a heart attack, stroke or other serious conditions can result in a significant level of disability, said Dr. Christopher Voscopoulos, medical director of Southern Hills Hospital and Medical Center’s intensive care unit.
“They are trading a very small risk (of contracting COVID-19) for a huge guaranteed risk of either death or disability,” Voscopoulos said.
He described hospitals as highly controlled environments with superior cleaning systems that have been improved since the COVID-19 pandemic began.
“In my opinion, you have a higher chance of getting COVID-19 in the community than you do in the hospital,” he said.
Unexplained declines
Visits by adults in to the emergency department at University Medical Center were down by more than 50 percent three weeks ago, but have since increased to about two-third of typical volumes, said Dr. Thomas Zyniewicz, an emergency medicine physician at UMC.
Some of the decline could be attributable to decreases in car accidents, since there are fewer drivers on the road, along with other side effects of social distancing. Then, too, those with relatively minor aches and pains may be avoiding hospitals for fear of COVID-19, he said.
Less neatly explained are declines, and not simply delays, in visits by patients with conditions that quickly can prove to be fatal.
Zyniewicz, a vice president with US Acute Care Solutions, said visits that result in a diagnosis of a heart attack have been down 41 percent, and of stroke by 36 percent, across the network of more than 200 hospitals served by the physicians group, including UMC.
Patients might delay going to the hospital on Christmas, but typically will flood the ER the next day, Zyniewicz said.
“Now we’re just having slow days,” he said, adding that the hospital has passed its peak for patients needing to be hospitalized for COVID-19.
Despite suggestions that fear of the new coronavirus may be keeping people away from the ER, there’s no evidence suggesting that more people are dying in their homes, Clark County Coroner John Fudenberg said on Friday.
“The data isn’t showing any unusual trends at this time,” he said.
For his part, Zyniewicz describes the decrease in true medical emergencies as a mysterious side effect of the pandemic.
It’s one that “no one has given a viable explanation for, and nor can I,” he said.
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.